6 Tips to Increase Your VA Rating for Migraines – The Definitive Guide

Today, we’re going in-depth to examine the VA rating for migraines. Migraine headaches are rated as follows: 0%, 10%, 30%, or 50%. The highest VA disability rating for migraines is 50%.
Brian Reese here, Air Force service-disabled veteran, VA disability expert, and founder of VA Claims Insider—the most trusted name in VA disability claims.
Now let me be clear about something veterans:
This is NOT your average “VA disability rating for migraines” predictions post.
Yes, I’ll cover the most important Migraine Headaches VA rating trends this year.
But you’re also going to get real BVA case law and cutting edge medical research studies that suggest a relationship between Migraine Headaches and various other service-connected disabilities.
So, regardless of your current VA disability rating for Migraines, this new guide will help you win, service connect, and get a higher VA rating for Headaches, regardless of previous denials.
- How to Get a 50% VA Rating For Migraines (NEW in 2020!)
- Chapter 1: Are Headaches a VA Disability?
- Chapter 2: The Term “Prostrating” Will Make or Break Your VA Claim for Migraines
- Chapter 3: VA Rating for Migraines Criteria
- Chapter 4: How to Get 50 VA Disability for Migraines
- Chapter 5: Expert Tips to Service Connect Your Migraines
- Chapter 6: List of VA Secondary Conditions Due to Migraines
- Migraines secondary to Tinnitus
- Migraines secondary to TBI
- Migraines secondary to TMJ
- Migraines secondary to PTSD
- Migraines secondary to Depression
- Migraines secondary to Anxiety
- Migraines secondary to Somatic Symptom Disorder
- Migraines secondary to Sinusitis
- Migraines secondary to Rhinitis
- Migraines secondary Cervical Strain (neck condition)
- Migraines secondary to Sleep Apnea
- Migraines secondary to Radiculopathy
- Migraines secondary to Asthma
- Migraines secondary to Medication Side Effects
- How to File a VA Claim for Migraines
- About the Author
How to Get a 50% VA Rating For Migraines (NEW in 2020!)
Chapter 1: Are Headaches a VA Disability?
Yes, headaches are a VA disability.
They fall under CFR 38, the Schedule for Rating Disabilities, diagnostic code 8100 for Migraines.
In fact, according to the Veterans Benefits Administration (VBA), and the Top 10 Most Common VA Disability Claims, Migraines are the #9 most commonly claimed VA disability.
Types of Headaches for VA Rating Purposes
While the law only specifically lists Migraines as a ratable VA disability condition, ANY type of headache condition can receive a VA rating if you have symptoms that affect your work, life, and functioning due to your military service or another service connected disability.
The International Headache Society and the Mayo Clinic have identified more than 150 different types of headaches, which are divided into three categories: Primary, Secondary, and Other.
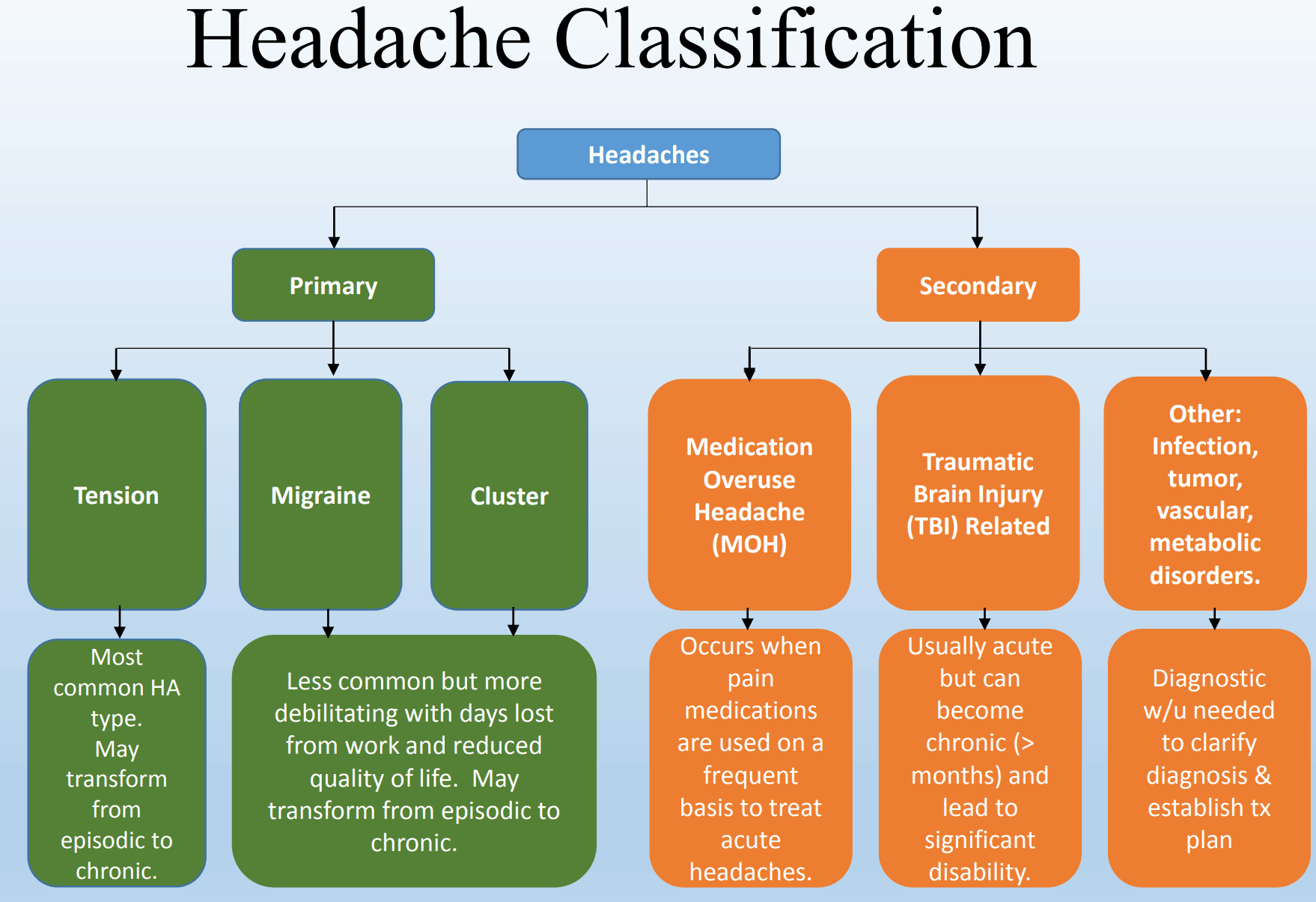
For example, Tension Headaches are the most common type of headaches among adults, and the most common type of headaches in veterans as well.
They cause mild to moderate pain and come and go over time.
They usually have no other symptoms.
Migraine Headaches are often described as pounding, throbbing pain.
They can last from 4 hours to 3 days and usually happen one to four times a month.
Along with the pain, people have other symptoms, such as sensitivity to light, noise, or smells; nausea or vomiting; loss of appetite; and upset stomach or belly pain.
Post Traumatic Headaches, for example, are quite common among veterans, specifically if you suffered from any type of head injury or trauma during military service.
Furthermore, post traumatic headaches, particularly migraine headaches, are commonly found in veterans who deployed in support of combat operations in Iraq and Afghanistan.
According to medical research, if you get a new headache within 7-10 days of your head injury or after you are conscious again from the trauma, you may have a condition known as a post-traumatic headache.
Chapter 2: The Term “Prostrating” Will Make or Break Your VA Claim for Migraines
What is a “Prostrating” Migraine Headache?
Perhaps the single most important term that can litterally make or break your VA rating for migraines is the word “Prostrating.”
The reason it’s so important is because the 30% and 50% VA ratings for Migraines contain the word “Prostrating” in reference to both frequency and severity of your condition.
What’s interesting is that neither VA regulations nor the Courts have attempted to define the term “Prostrating.”
By way of reference, according to MERRIAM WEBSTER’S COLLEGIATE DICTIONARY 999 (11th Ed. 2007), “Prostration” is defined as “Complete physical or mental exhaustion.”
A very similar definition is found in DORLAND’S ILLUSTRATED MEDICAL DICTIONARY 1554 (31st Ed. 2007), in which “Prostration” is defined as “Extreme exhaustion or powerlessness.”
The best definition we could find for “Prostrating” comes from Dictionary.com:
“To lay oneself flat on the ground face downward, especially in reverence or submission.”
Prostrating is further defined as weakness, fatigue, distress, exhaustion, illness, or functional loss, for example:
“To reduce (someone) to extreme physical weakness.”
Statement in Support of a Claim for Migraines Example
Veterans listen up to these Migraines Buddy Letter examples and write them down!
In the absence of service treatment records or current symptoms of Migraine Headaches, you can get a competent and credible Buddy Letter from a first-hand witness as to the frequency and severity of your Migraines.
A high-quality Buddy Letter from a first-hand witness can help you win, service connect, and get a higher VA rating for migraines in less time!
The best word combinations for your Statement in Support of a Claim for Migraines, a Buddy Letter for Migraines, what you tell your VA doctor, or how you should describe your Headaches at a Migraines VA C&P Exam go something like this, assuming you really do have severe symptoms:
“My headaches are so severe, that when I get an attack, which happens 3-4 times per week, I end up having to lie down in a dark room for hours until they stop. This has affected my work, life, and social functioning. In fact, I’m now unemployed because I couldn’t perform the functions of my job due to the severity and frequency of my headaches.”
“My migraines cause extreme radiating pain from my neck all the way up through both sides of my head. When I’m having a migraine, I end up taking sick leave from work because I must lie down by myself in a quiet room.
Chapter 3: VA Rating for Migraines Criteria
CFR 38, Part 4, the Schedule for Rating Disabilities, lists Migraines under code 8100.
The Migraines VA rating scale for 2020 consists of four rating possibilities ranging from 0 to 50: 0%, 10%, 30%, and 50%.
The symptoms become markedly more severe between at the 30% and 50% rating levels, as evidenced by the rating criteria below:
| 8100, Migraine: | Rating |
| Migraines with very frequent completely prostrating and prolonged attacks productive of severe economic indaptability | 50% |
| Migraines with characteristic prostrating attacks occurring on an average once a month over last several months | 30% |
| Migraines with characteristic prostrating attacks averaging one in 2 months over last several months | 10% |
| Migraines with less frequent attacks | 0% |
Chapter 4: How to Get 50 VA Disability for Migraines
There is a significant different between the 30% rating for Migraines and the 50% rating for Migraines.
For example, look at this real denial letter from a VA Rater, for a veteran who was already ready at 30% for migraines, but was seeking an increase to 50% for migraines:
“Although the medical evidence shows that the frequency of the headaches has increased, there is no objective medical evidence showing that these headaches are at all prostrating in nature which would affect economic inadaptability. However, based on the totality of the evidence which includes the veteran’s subjective statements, and resolving all reasonable doubt in his favor, we feel that the 30% rating threshold has been met justifying an increase at this time. A higher evaluation is not warranted unless the objective medical evidence shows very frequent, completely prostrating, and prolonged attacks productive of severe economic inadaptability.”
Medical Evidence Requirements for Migraines
The denial states the medical evidence did NOT show prostrating headaches or economic loss.
If you think you deserve a higher VA rating for Migraines, you need to have medical evidence that discusses the severity of your headaches, whether they are prostrating in nature, and if these headaches affect your work.
The best way to do this is to get a DBQ for Migraines completed from a qualified medical professional.
If you’re already service-connected for Migraines at 0% or higher, this is a simple increase based upon new and relevant medical evidence (the DBQ report).
Sometimes, a VA Rater will accept a Migraines DBQ on its own and grant the rating increase without a C&P exam.
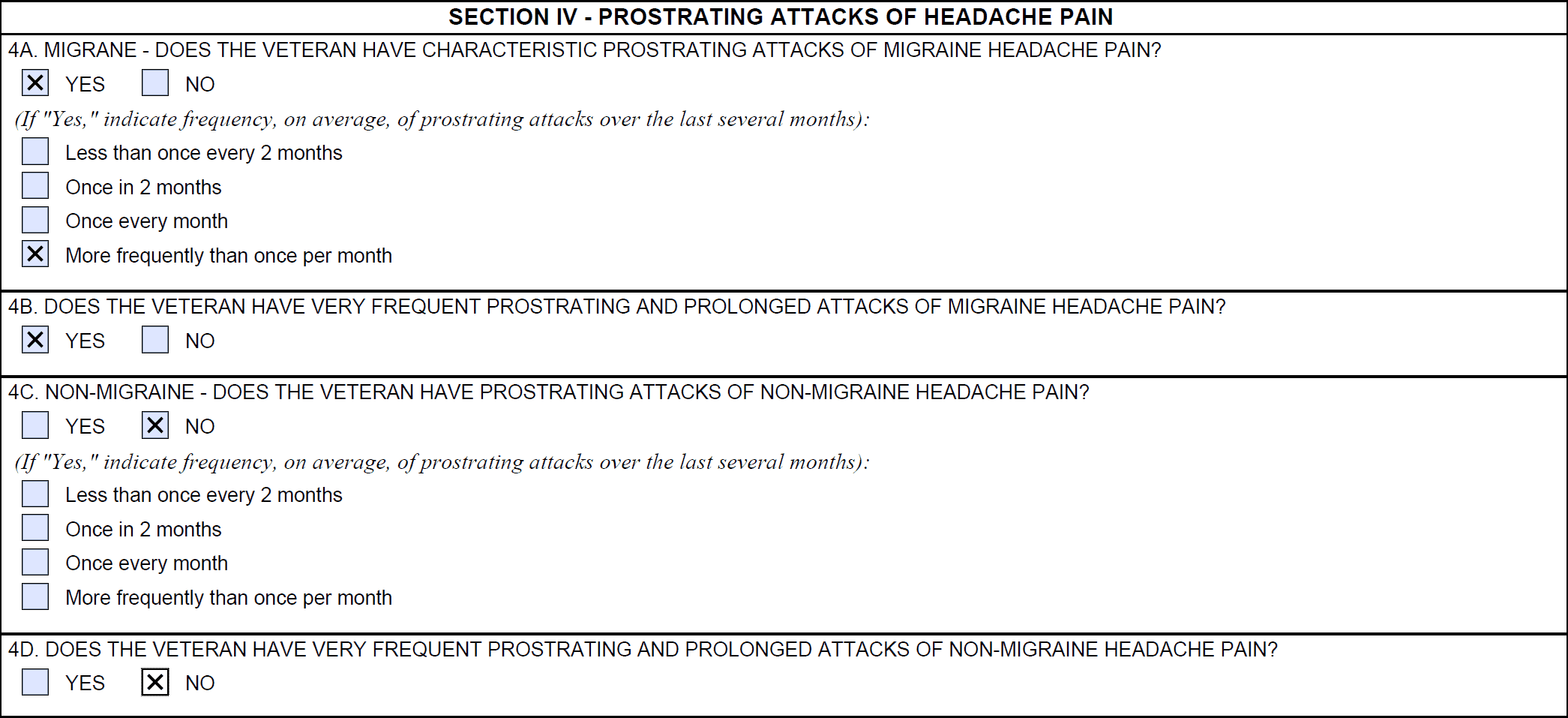
The most important section of the DBQ for Migraines is Section IV – Prostrating Attacks of Headache Pain.
If your Migraines are so severe that you often need to lie down in a dark room for hours, which indicates “Prostrating” attacks, make sure to tell your doctor about it, and ensure the DBQ is completed correctly.
Another tip for Migraines is you need to be documenting the frequency and severity of your migraines over the past several months, so you have additional evidence.
You can use apps on your smartphone, such as the Migraine Buddy App, which you can then download the daily and monthly reports to use in support of your VA claim for headaches.
30% VA Rating for Migraines
At the 30% VA rating for Migraines, the law lists headaches “with characteristic prostrating attacks occurring on an average once a month over last several months.”
Note the keyword of “prostrating,” meaning you’ve had to lie down.
You can also see that the 30% rating has prostrating attacks that occur roughly one time per month over the past several months.
There is no mention of any functional or economic loss.
50% VA Rating for Migraines
At the 50% VA rating for Migraines, the law describes headaches “with very frequent completely prostrating and prolonged attacks productive of severe economic inadaptability.”
Note the keywords of “very frequent completely prostrating,” meaning you’ve had to lie down more often, and the Migraines could last for extended periods of time.
You can also see that the 50% rating introduces “severe economic inadaptability.”
Regarding the term “productive of economic inadaptability,” the case law precedent indicates that “productive of” can also be read as having either the meaning of “producing” or “capable of producing.”
Further, the term “inadaptability” has NEVER been defined by the courts, nor can a definition be found anywhere in 38 CFR.
We do know, however, that the term “severe economic inadaptability” refers to a veteran’s inability to work, but NOTHING in the Migraines Diagnostic Code 8100 requires that the veteran be completely unable to work in order to qualify for a 50% rating.
Therefore, a veteran can qualify for a 50 percent VA rating for Migraines and still be working or able to work.
For example, maybe you’ve been fired from a job because you missed work so often due to the severity of your Migraines.
Perhaps you have severe Migraines on a weekly basis, and you’ve used all your sick leave at work and it’s now affecting your ability to produce and earn a living, but you’re still working.
Chapter 5: Expert Tips to Service Connect Your Migraines
Many veterans unsuccessfully attempt to service connect Migraines as a primary disability seeking direct service connection.
The problem is you probably weren’t diagnosed with Migraines while on active duty and it’s now years later, meaning it will be difficult to prove direct service connection.
But maybe there’s a better way?
There is!
And it’s an expert level tip from Brian Reese and the VA Claims Insider medical team.
Migraines and Secondary Service Connection
Migraines, and many other types of headaches, can be medically linked to numerous other service-connected disabilities.
Thus, it’s very possible for veterans to seek service connection on a secondary basis, which requires a showing of causation.
A showing of causation requires that the secondary disability be shown to be “proximately caused by” or “proximately aggravated by” another service-connected disability.
Accordingly, service connection may be granted on a secondary basis for a disability that is proximately due to, the result of, or aggravated by a service-connected disability. See 38 C.F.R. § 3.310(a) and (b) (2014). Also see Allen v. Brown, 7 Vet. App. 439, 448 (1995).
By law, there are three essential elements that must be satisfied for Migraines as a secondary condition to prove secondary service connection:
- A medical diagnosis of Migraines or any other type of headache condition
- Evidence of a service-connected primary disability (such as TBI, Tinnitus, PTSD, Depression, Anxiety, Sinusitis, Rhinitis, Cervical Strain), AND
- Medical nexus evidence establishing a connection between the current disability (Migraines) as proximately due to, the result of, or aggravated by another service-connected disability rated at 0% or higher.
The first part can be satisfied with any existing medical evidence in service treatment records, VA medical records, or any private medical records.
The second part can be satisfied with a veteran’s existing service-connected disability rated at 0 percent or higher.
The third part can be satisfied with a Medical Nexus Letter from a qualified medical professional.
>> If you need a Medical Nexus Opinion to help service connect your VA disabilities, please click HERE to join our premier membership program, VA Claims Insider Elite.
Chapter 6: List of VA Secondary Conditions Due to Migraines
Headaches are often granted secondary service connection because the disability (Migraine Headache) is shown to be proximately due to, the result of, or aggravated by another service-connected disability.
The frequency and severity of Headache Conditions typically increases with the severity of other service-connected disabilities.
For example, veterans with more severe PTSD symptoms are likely to have more severe Migraine Headache symptoms, suggesting a correlation between the two.
There are many possible links for veterans to establish secondary service connection for Migraines, including, but not limited to:
Migraines secondary to Tinnitus
Research suggests that there is a connection between Headaches and Tinnitus and the symptoms go hand in hand with many types of headaches, including migraines and hypertension. Recent results show 27% of Tinnitus sufferers also suffer from headaches. Thus, there is a clear medical etiology to suggest that Migraines and many types of Headaches can be proximately due to or aggravated by Tinnitus, aka, ringing in the ear syndrome.
Migraines secondary to TBI
There are several research studies linking Traumatic Brain Injury (TBI) to Migraines as well as post traumatic headaches. A 2012 study of soldiers returning from combat found that chronic daily headache was “considerably more common” than might be expected. For example, one study concluded that 29% of soldiers who deployed and suffered from mild TBI also had Migraines.
Migraines secondary to TMJ
Research has shown that people who grind or clench their teeth are more likely to have Migraines than those who don’t. Thus, there is a medical link between Migraines and TMJ or TMD. A similar body of research suggests that the trigeminal nerve plays an important role in the start of a Migraine attack. The trigeminal nerve sends signals to the blood vessels and lining of the brain, leading to cortical spreading depression and a release of chemicals that result in the pain and throbbing of a Migraine Headache. Further, neck and jaw problems are a common cause of Migraine Headaches. Here’s a 2011 BVA case that granted Migraine Headaches secondary to TMJ.
Migraines secondary to PTSD
Research suggests a connection between Migraines and Post Traumatic Stress Disorder, especially in military veterans. When it comes to headaches, patients with migraine or tension headaches report high rates of exposure to traumatic events. In addition, about 17% have symptoms consistent with a PTSD diagnosis. PTSD can significantly interfere with many aspects of a veteran’s life, including work, life, and social functioning. This fact likely causes more stress, which increases the likelihood of headaches.
Here’s an example of a BVA case decision from 2015 that granted secondary service connection for Migraine Headaches secondary to PTSD. Interestingly, the VA C&P examiner concluded it was less likely than not that the Veteran’s headaches are proximately due to or aggravated by his PTSD. However, the veteran had two positive medical nexus opinions from private providers, that it was “more likely than not” that the headaches were a result of the PTSD. Thus, in view of the totality of the evidence, the Board finds that the evidence is at least in “equipoise” as to whether the Veteran’s current headaches are proximately due to his PTSD. Accordingly, entitlement to service connection for headaches, as due to service-connected PTSD, is granted.
Migraines secondary to Depression
There is a growing body of evidence that suggests a link between Migraines, headaches, and Depression although it’s not entirely clear as of 2019. The most likely link to help a veteran connect Migraines secondary to Depression is through an “interim link,” meaning Migraines that are proximately due to or aggravated by service connected Depression, specifically, the side effects of medications a veteran is taking to manage the symptoms of Depression. Many SSRIs have serious side effects, including nausea, vomiting or diarrhea, migraines and other types of headaches, drowsiness, dry mouth, insomnia, nervousness, agitation or restlessness, dizziness, sexual problems, such as reduced sexual desire, difficulty reaching orgasm or inability to maintain an erection (erectile dysfunction), and impact on appetite, leading to weight loss or weight gain.
Migraines secondary to Anxiety
Researchers have suggested that a common link exists between Anxiety Disorders and Migraines. Migraines and chronic daily headaches are common in people who suffer from anxiety disorders, especially in veterans who are already service connected for a mental health condition, such as PTSD, depression, and anxiety. Many studies have found that people with Generalized Anxiety Disorder (GAD) and panic disorder experience Migraines or other types of Headaches at a much higher rate than those without a mental health condition. Again, in our experience, the best way to service connect Migraines secondary to Anxiety is through the interim medical side effects link listed above.
Migraines secondary to Somatic Symptom Disorder
There is a strong medical link between Migraines and Somatic Symptom Disorder. One study concluded, “Associated somatic symptoms are more common in patients with Migraines, with more frequent severe headaches, and with associated anxiety or depression.” Headache disorders may be characterized as showing increasing somatic prevalence as headaches become more frequent.
Migraines secondary to Sinusitis
A growing body of research links Migraines to sinus conditions such as Sinusitis. In the recent American Migraine Study II, 40% to 70% of respondents with Migraine Heads had comorbid allergies, meaning they occurred together. Research studies show how common sinus symptoms occur with migraine. Specifically, in one such study, 45% of patients with Migraines had symptoms of Sinusitis, such as head and nose pressure and pain, nasal congestion, and runny nose.
Migraines secondary to Rhinitis
Research studies have concluded that people with Rhinitis are more than ten times more likely to have Migraines. Thus, there is a very strong link associated with Migraines secondary to Rhinitis. Some studies have shown that up to 90% of Sinus Headaches are actually Migraines.
Migraines secondary Cervical Strain (neck condition)
The most common symptoms of cervical disorders, such as cervical strain is suboccipital cervicogenic headache and ongoing or motion-induced neck pain. Thus, there is a medical nexus link connecting Migraines secondary to Cervical Strain. Here’s a recent BVA case from 2015 that granted Occipital Headaches secondary to cervical spine Degenerative Disc Disease (DDD).
Migraines secondary to Sleep Apnea
Headaches have been medically linked to patients who suffer from moderate to severe sleep apnea, especially when oxygen levels drop due to the intermittent breathing from Obstructive Sleep Apnea (OSA). Sleep apnea causes air to be trapped in the lungs, and this de-oxygenated air is the waste product carbon dioxide. This lack of oxygen in the bloodstream, along with carbon dioxide, negatively affects the brain and leads to headaches, which can also be Migraines.
Migraines secondary to Radiculopathy
Medical research shows a strong correlation between Migraines and Radiculopathy, especially when the upper nerve roots are involved. Patients have reported this pinched nerve in the neck leads to more serious headaches, such as Migraines. It should be noted, however, that headaches caused by lower nerves in the neck are more common than upper nerve related headaches.
Migraines secondary to Asthma
There is a strong correlation between Migraines and Asthma. One research study reported that people with Migraines are 2 to 3.5 times more likely to have or develop Asthma.
Migraines secondary to Medication Side Effects
Literally thousands of over the counter medications and prescription medications, especially Selective Serotonin Reuptake Inhibitors (SSRIs) can cause or make Migraines and Headaches in general, worse. If you’re a veteran who takes medications to help manage the daily chronic pain or mental health conditions you suffer from due to service, and you now have Headaches, you can likely get service connected for the Migraines secondary to the side effects of the medications.
How to File a VA Claim for Migraines
About the Author
Brian Reese is nationally recognized VA disability expert and thought leader.

His frustration with the 8-step VA disability claims process led him to create “VA Claims Insider,” which provides U.S. military veterans with FREE high-value resources for successfully submitting or re-submitting a winning VA disability compensation claim.
He is also the CEO of Military Disability Made Easy, which is the world’s largest free searchable database for all things related to DoD disability and VA disability claims and has served more than 4,000,000 military members and veterans since its founding in 2013.
His eBook, the “9 Secrets Strategies for Winning Your VA Disability Claim” has been downloaded more than 300,000 times in the past three years and is the #1 rated free VA disability claims guide for veterans.
He is a former active duty Air Force officer with extensive experience leading hundreds of individuals and multi-functional teams in challenging international environments, including a combat tour to Afghanistan in 2011.
Brian is a Distinguished Graduate of Management from the United States Air Force Academy, Colorado Springs, CO and he holds an MBA from Oklahoma State University’s Spears School of Business, Stillwater, OK, where he was a National Honor Scholar (Top 1% of Graduate School class).

